Author: Tanya Washington Stephens, MD,Assistant Professor of Diagnostic Imaging, Assistant Professor ofDiagnostic Radiology, Section of Breast Imaging, University of Texas MDAnderson Cancer CenterCoauthor(s): Gary J Whitman, MD, Associate Professor, Department of Radiology, The University of Texas MD Andersen Cancer Center
Updated: May 12, 2009Introduction
Role of the radiologist
Radiologistswho interpret mammograms encounter calcifications on a daily basis.Most of the breast calcifications encountered by radiologists arebenign. Radiologists must be able to identify typically benign breastcalcifications that do not require biopsy to prevent unnecessaryprocedures and to reduce patient anxiety.1,2,3,4
Typically,benign calcifications that do not require biopsy are skin or dermalcalcifications, vascular calcifications, lucent-centeredcalcifications, eggshell or rim calcifications, coarse or popcornlikecalcifications, large rodlike calcifications, round and punctuatecalcifications, milk of calcium calcifications, suture calcifications,and dystrophic calcifications.5,6
Distribution of breast calcifications
Breast calcifications are described in terms of type and distribution and categorized according to the Breast Imaging Reporting and Data System (BI-RADS) of the American College of Radiology (ACR).7,8,9,10,11
Distributionmodifiers (grouped or clustered, linear, segmental, regional, diffuse)are used to describe the arrangement of the calcifications.Historically, the terms grouped or clustered wereused to describe suspicious calcification. Now, these terms are neutraland may be used to describe benign or malignant processes. Grouped or clustered should be used to describe calcifications that occupy a small volume (<2 µL) of tissue.12
Calcifications that are linearly distributed are arranged in a line and may have branch points.
Segmentallydistributed calcifications suggest deposition of calcification in aduct and its branches. This type of calcification may be secondary tobenign or malignant processes.
Regionally distributedcalcifications are most likely due to benign processes. Thesecalcifications are scattered in a large volume of the breast and do notnecessarily conform to a ductal distribution.
Diffusely distributed calcifications are scattered randomly throughout the breast.
ACR BI-RADS to describe breast calcifications
TheACR BI-RADS lexicon enables radiologists to use similar terminology todescribe mammography findings. This lexicon facilitates data trackingand provides clear management and follow-up recommendations toreferring physicians, allied healthcare providers, and patients. Thereare 7 ACR BI-RADS standardized categories.8,9
Category0, or "need additional imaging evaluation," is used if additionalimaging is needed. This category is almost always used in a screeningsituation and should be used only rarely after a full imaging workup.Additional imaging evaluation includes the use of spot compression andmagnification views, along with other tailored mammographic views andultrasonography.
Category 1, or "negative," is used if there areno findings to comment on. For example, the breasts are symmetrical,and no masses, architectural disturbances, or suspicious calcificationsare present.
Category 2, or "benign finding(s)," is used if theradiologist wishes to describe a benign finding while still concludingthat there is no mammographic evidence of malignancy.
Category 3,or "probably benign finding–initial short-interval follow-upsuggested," is used when a noted finding has a very high probability ofbeing benign. The finding is not expected to change over the follow-upinterval, but the radiologist prefers to establish its stability overtime.
Category 4, or "suspicious abnormality–biopsy should beconsidered," is used when a finding has a definite probability of beingmalignant.
Category 5, or "highly suggestive ofmalignancy–appropriate action should be taken," is used when a findinghas a high probability of being cancerous.
Category 6, or"know biopsy-proven malignancy-appropriate action should be taken," is"reserved for lesions identified on imaging study with biopsy proof ofmalignancy prior to definitive therapy."
Typically, benigncalcifications will be placed in ACR BI-RADS categories 1 and 2.Sometimes, these calcifications are initially placed in ACR BI-RADScategory 0 and, after additional imaging evaluation, are found to havebenign features. Early in their development, calcifications (eg,vascular, dystrophic, or lucent centered calcifications) may beindeterminate; these are often followed at short intervals to establishor confirm their etiology (ie, BI-RADS category 3).
Pathophysiology:Calcium is a silver-white bivalent metallic element of the alkalineearth group. Calcifications result from the deposition of calcium saltsin tissues.
Frequency:
- In the US: Benign calcifications may be identified in women of any age or race.
- Internationally: Benign calcifications may be identified in women of any age or race.
Mortality/Morbidity:
- Benign calcifications are not lethal.
- Morbidity may occur with unnecessary biopsy.
Race: Benign calcifications may be identified in women of any age or race.
Sex: Benign calcifications may be identified in women of any age or race.
Age: Benign calcifications may be identified in women of any age or race.
Clinical Details: Calcified siliconomas, calcified paraffinomas, fat necrosis, degenerating fibroadenomas, and dystrophic calcifications may be palpable on physical examination.
Preferred Examination: High-quality mammographyis the best diagnostic tool for the identification of breastcalcifications. Accredited, dedicated mammographic equipment should beused to obtain high-quality images. Mammography technologists must bewell trained and skilled in the proper positioning and compression ofthe breast.
Mammograms should always be interpreted on dedicatedhigh-luminance mammographic view boxes or viewers, and a magnifyingglass should be used routinely. Extraneous light and glare should beeliminated for optimal viewing conditions. Mammograms should bearranged in the same manner at each interpretation session to minimizeleft-right confusion.
Routine mammograms should includecraniocaudal (CC) and mediolateral oblique (MLO) views. That is, the 2mammographic views usually obtained first for screening or diagnosticevaluations are the MLO view and the CC view. Magnification images ofcalcifications should be obtained in the CC and mediolateral (ML) orlateromedial (LM) views, also known as true lateral views. Tangentialviews are useful for verification of the intradermal location ofcalcifications.
Comparing current mammograms with priormammograms is essential to determine the stability of anycalcifications detected. Finally, on the basis of the interpretation,the radiologist can make an informed decision about whether thecalcifications identified are benign and do not require biopsy orwhether the appearance of the calcifications warrants biopsy.
Limitations of Techniques:Mammography is limited in evaluating benign calcifications when benigncalcifications morphologically overlap with indeterminate or malignantcalcifications. These calcifications may be observed for a short period(ACR BI-RADS category 3), or biopsy may be performed (ACR BI-RADScategories 4 and 5).
Patient Education: For excellent patient education resources, visit eMedicine's Imaging Center, Cancer and Tumors Center, and Women's Health Center. Also, see eMedicine's patient education articles Mammogram, Breast Lumps and Pain, and Breast Self-Exam.
Differentials
Indeterminate calcifications
Malignant calcifications
Mammogram
Skin or dermal calcifications
Skin or dermal calcifications (see Image 1)are usually identified as spherical, lucent-centered calcifications atthe periphery of the breast, especially in the inferior, posterior, andmedial aspects.13,14 Skin calcifications may develop from a degenerative metaplasticprocess. Usually, skin calcifications are readily distinguished asbenign findings. However, in some cases, additional imaging is neededto differentiate skin calcifications from more worrisome calcifications.
Multiple skin calcifications (arrows).
Whenmammograms are compared, calcifications that maintain a fixedrelationship to one another are suggestive of a dermal location.Magnification views may be used to demonstrate the lucent centerscharacteristic of skin calcifications. In some cases, a skinlocalization procedure may be needed to prove that the calcificationsare in the skin.
When performing a skin localization procedure, theradiologist should determine if the calcifications are more likely tobe in the upper or the lower portion of the breast. Thereafter, thepatient's breast is placed in the mammographic unit by using afenestrated compression device. For calcifications presumed to be inthe upper part of the breast, a CC approach is used with thefenestration device in the region of the calcifications. Forcalcifications thought to be in the inferior part of the breast, acaudocranial approach is used. A metal marker is then placed over thecalcifications, and a tangential view is obtained to show the dermalcalcifications in the skin.
Vascular calcifications
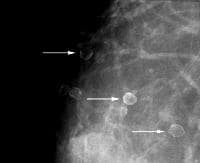
Vascular calcifications (see Image 2)are commonly identified on mammography, especially in older women.Vascular calcifications, which are usually secondary to medialatherosclerosis, often demonstrate a characteristic train tracklikeconfiguration. In some cases, it may be difficult to distinguishvascular calcifications from ductal calcifications (includingcalcifications representing ductal carcinoma in situ). Arterialcalcification in the breasts may be associated with diabetes andhyperparathyroidism.
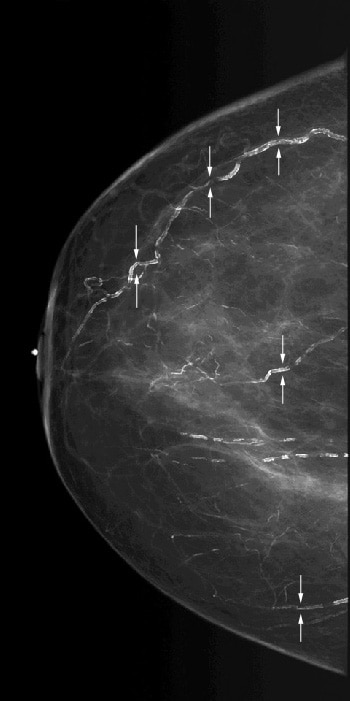
Scattered vascular calcifications with train track—like appearance (arrows).
Thepresence of mammary vascular calcifications may allow for the detectionof women with elevated cardiovascular disease risk profiles.15,16,17,18 Researchers in the Netherlands examined 12,239 women in apopulation-based breast cancer screening program. The study showed asignificant correlation between vascular calcifications identified onmammography and myocardial infarction, transient ischemic attacks, and hypertension.Additional studies are needed to validate the potential role forscreening mammography in the early detection of women at risk forcardiovascular disease.Lucent-centered calcifications
Lucent-centered calcifications (see Images 3-5),which are round or oval, are almost always benign and they have thickerwalls than those of rim or eggshell calcifications. Skin calcificationsare often lucent-centered, and lucent-centered calcifications may formaround benign debris in the ducts. Other entities that may appear aslucent-centered calcifications on mammography include siliconegranulomas and fat necrosis.
This patient was in a car accident and sustained a seatbelt injury. The lucent-centered calcifications seen are typical of fat necrosis.
This patient underwent breast-conserving surgery. The lucent-centered calcifications (arrow) are typical of fat necrosis.
Multiple silicone granulomas are lucent-centered calcifications.
Fatnecrosis results from several causes including trauma, surgery, andradiation therapy. Fat necrosis occurs most often in fatty pendulousbreasts of middle-aged women. Lucent-centered calcifications may resultfrom fat necrosis, and the thickness of the calcified wall around thelucent area is variable and probably related to the amount ofdesmoplastic reaction.Eggshell or rim calcifications
Eggshell or rim calcifications (see Image 6)are thin and appear as calcium deposited on the surface of a sphere.The walls of eggshell or rim calcifications are thinner than the wallsof lucent-centered calcifications.
Eggshell or rim calcifications (arrows) have walls thinner than those of lucent-centered calcifications.
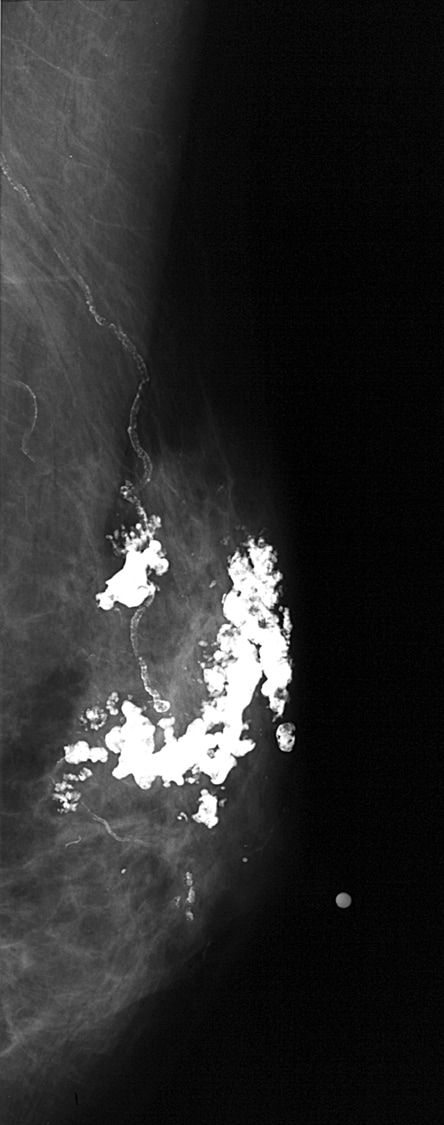
Coarse or popcornlike calcifications
Coarse or popcornlike calcifications (see Images 7-8) are associated with the involution and hyaline degeneration of fibroadenomas. Fibroadenomas are the most common breast masses seen in women younger than 35 years of age.
This mass with associated large, coarse calcifications (arrows) is a degenerating fibroadenoma.

Calcifications associated with fibroadenomas have been termed popcorn calcifications because of their large size and dense, coarse appearance.
Large rodlike, or secretory calcifications
Large rodlike or secretory calcifications (see Image 9) are oriented along the axes of the ductal system. These calcifications result from calcification of ductal secretions.
Large rodlike or secretory calcifications are oriented along the axis of the breast ductal system.
Largerodlike calcifications may have lucent centers if the ductal secretionsundergo peripheral calcification. In general, these calcifications arecoarser and larger (usually > 1 mm in diameter) than malignantcalcifications. Large rodlike calcifications are commonly bilateral anddiffuse. These calcifications are associated with secretory disease,plasma cell mastitis, and duct ectasia.Round and punctate calcifications
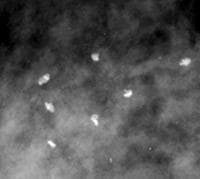
Punctate calcifications (see Image 10) are spherical calcifications that have well-defined margins.
Scattered round and punctate calcifications (arrows).
Punctatecalcifications usually measure less than 0.5 mm in diameter. Roundcalcifications are benign spherical calcifications that may vary insize. When less than 1 mm, round calcifications are frequently formedin the acini of the lobules.Milk of calcium
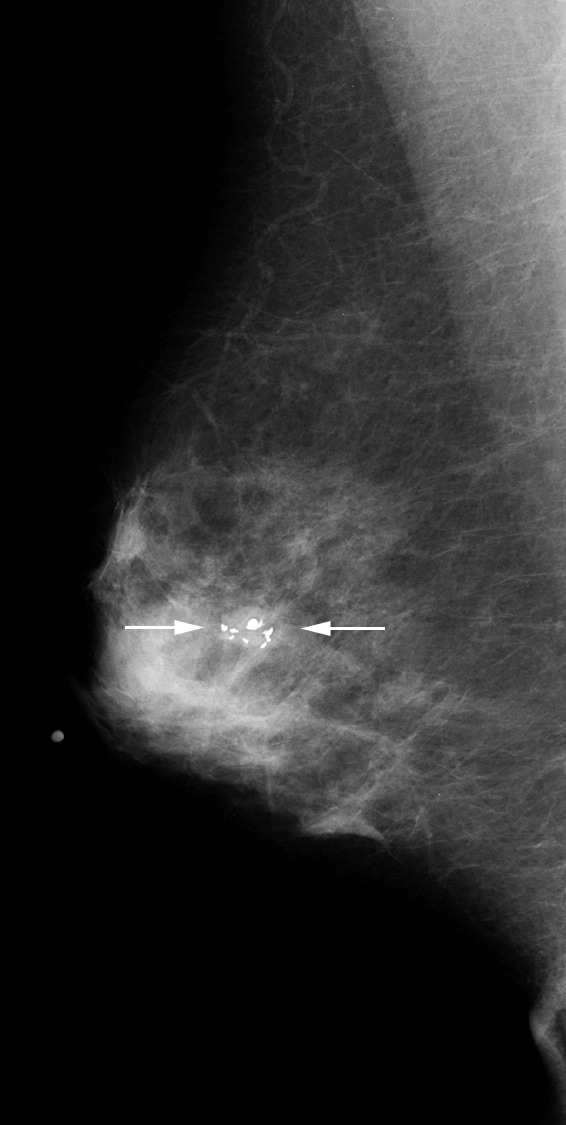
Milk of calcium (see Image 11)is a benign process that can be diagnosed readily during mammography,especially with magnification views in the CC and the true lateral (MLor LM) projections.19
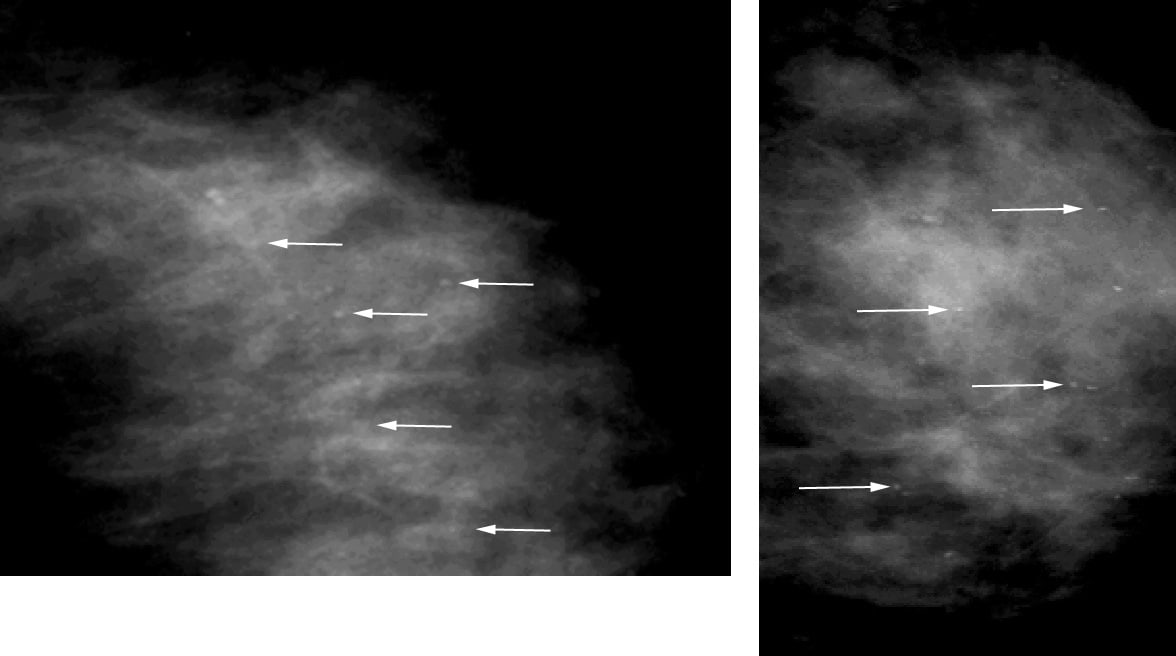
Left, On the craniocaudal (CC) magnification view, milk of calcium appears poorly defined and smudgy (arrows). Right, On the mediolateral (ML) or the lateromedial (LM) magnification view, milk of calcium is seen as sharply defined, crescent-shaped, semilunar, curvilinear (concave up), or linear arrangements (arrows).
Whenmilk of calcium is imaged with a vertical x-ray beam on the CC view,the calcifications appear poorly defined and smudgy. When imaged with ahorizontal x-ray beam on the ML or the LM view, the calcifications areseen as sharply defined, crescent-shaped, semilunar, curvilinear(concave up), or linear arrangements. The characteristic appearance ofthe calcifications on the magnification views helps to establish thecorrect diagnosis of milk of calcium.Suture calcifications
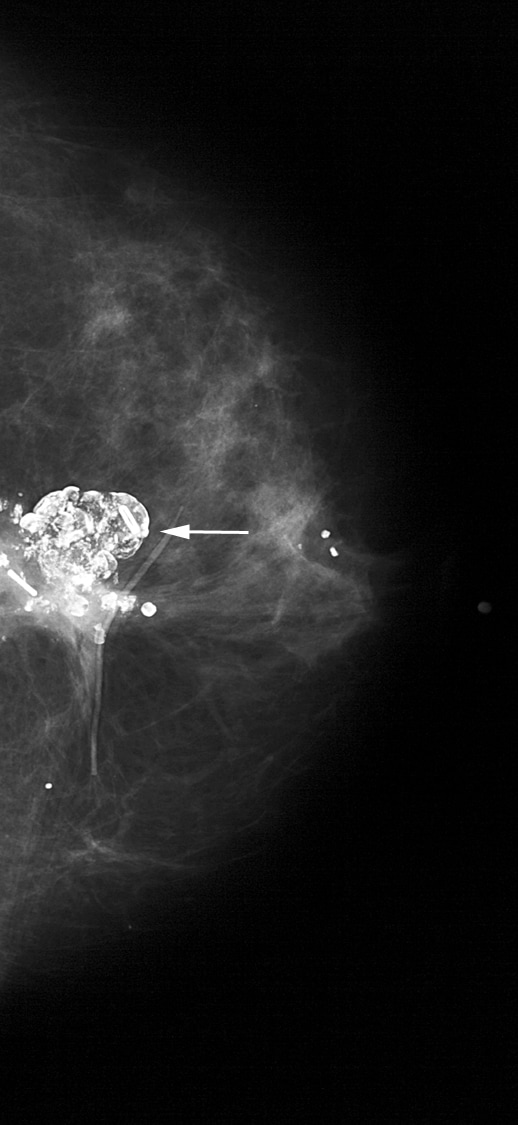
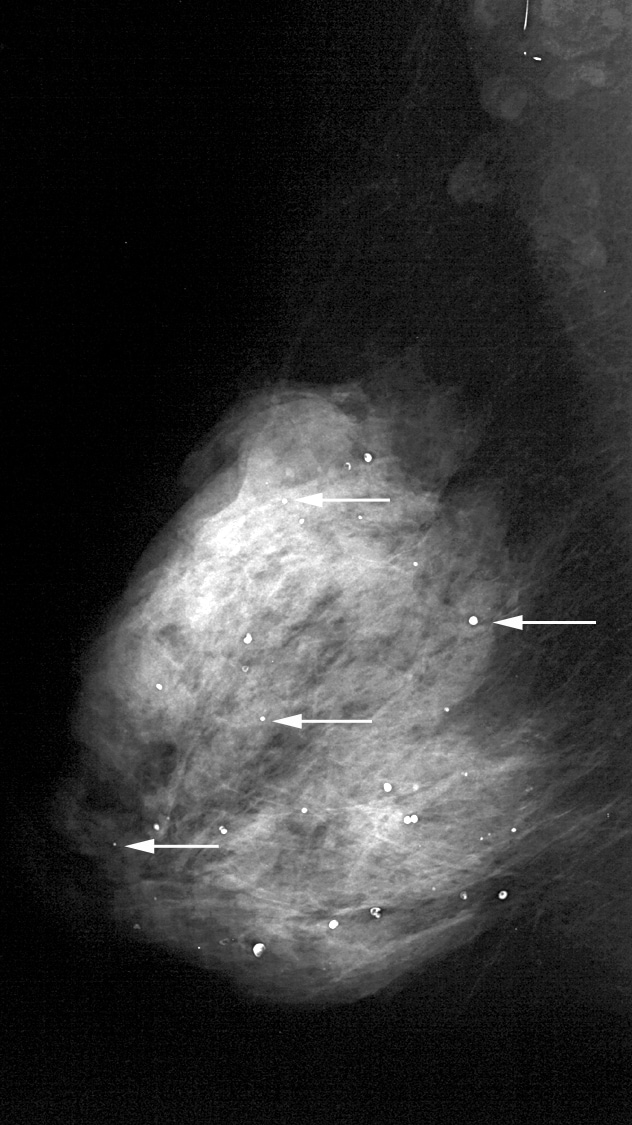
Suture material (see Image 12) may become calcified, resulting in suture calcifications.20,21 Suture calcifications are usually seen at a known surgical site, andthe calcifications may be linear or tubular. Knots may be demonstrated.Suture calcifications are likely due to delayed resorption of catgutsutures, which can provide a matrix on which calcium can precipitate.
Knotted suture calcifications.
Dystrophic calcifications
Dystrophic calcifications (see Image 13) may form secondary to trauma, surgery, or irradiation.
This patient's breast was burned. The irregular, large calcifications are dystrophic.
Most often irregular, dystrophic calcifications are usually larger than 0.5 mm, and they may have lucent centers.
Intervention
Typically,benign calcifications do not require intervention. The correctdiagnosis of benign calcifications can prevent unnecessary biopsy andsurgical inventions.
References: http://www.medscape.com/medline/abstract/414533